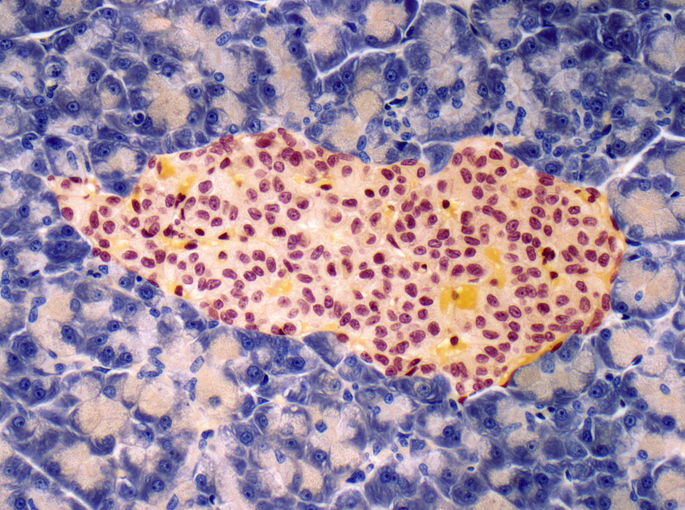
A recent study from the Perelman School of Medicine at the University of Pennsylvania and Harvard University reveals that an ultrathin, flexible electronic mesh can enhance the maturation of pancreatic islet cells, potentially transforming diabetes care. The research, published in Science, demonstrates how this mesh can be integrated into developing pancreatic tissue to deliver rhythmic electrical pulses, guiding stem-cell-derived islet cells toward functional maturity. This innovative approach may pave the way for generating viable human islets, addressing the critical shortage of donor organs for diabetes patients.
Type 1 diabetes, affecting approximately two million Americans, leads to the destruction of insulin-producing pancreatic islets. Current treatment options remain limited, as lab-grown islet cells often fail to mature adequately, hindering their ability to regulate blood sugar effectively. The researchers’ findings suggest that electrical stimulation can not only enhance individual cell functionality but also promote synchronization among cells, a crucial factor for effective glucose control.
Looking forward, the potential applications of this technology are significant. The team envisions that lab-grown islet cells could be electrically stimulated before transplantation or that the mesh could serve as a long-term monitoring device, adapting to cellular needs autonomously. This research not only sheds light on islet biology but also hints at a future where electronics and biology converge to improve diabetes management.
Get started today with Solo access →